Background: Evaluation of MRD is standard in patients with AML. However, the role of decentralized MRD assessment for risk stratification in AML remains largely unknown, and so it does which methodological aspects are critical to empower the evaluation of MRD with prognostic significance, particularly if using MFC.
Aim: To evaluate the role of decentralized MRD assessment using MFC for risk stratification and putative treatment individualization of patients with AML.
Methods: This study was performed on 1,076 AML patients in complete remission (CR) after 7+3 induction chemotherapy, in whom MRD was evaluated by MFC in local laboratories over a period of 20 years in the PETHEMA group. We conducted a survey of technical aspects of MFC based MRD testing in the laboratories of the 60 participating Hospitals, to determine the impact of methodological heterogeneity in the prognostic value of MFC.
Results: We first investigated the most effective MRD cutoff to stratify patients' risk at first remission. Patients were segmented into progressively higher cutoffs, starting at 0.01% followed by 0.05%, 0.1%, 0.5% and 1%. Our results showed that 0.1% reached higher statistical significance to discriminate patients with different relapse-free survival (RFS, HR: 0.77; P = .001) and overall survival (OS, HR: 0.73; P = .001). In multivariate analyses together with patients' age, WBC, genetic risk and post-consolidation therapy, MRD status was selected as an independent prognostic factor for OS. To further define the utility of "real-world" MRD assessment using MFC in risk stratification of AML, recursive partitioning was performed using the prognostic and treatment related factors selected in the multivariate Cox model for OS. Of the four variables evaluated, hematopoietic stem cell transplantation (HSCT, regardless of autologous or allogeneic source) vs no transplant emerged as the best single discriminator for OS, followed by genetic risk, age and MRD status. There were two branching points defined by MRD status; the first in patients ≤60 years with intermediate genetic risk who were not transplanted and the second in patients with adverse genetics who were not transplanted, in whom <0.1% MRD faintly improved the dismal outcome of this subgroup. Overall, patients not referred to HSCT had dismal RFS regardless of MRD levels.
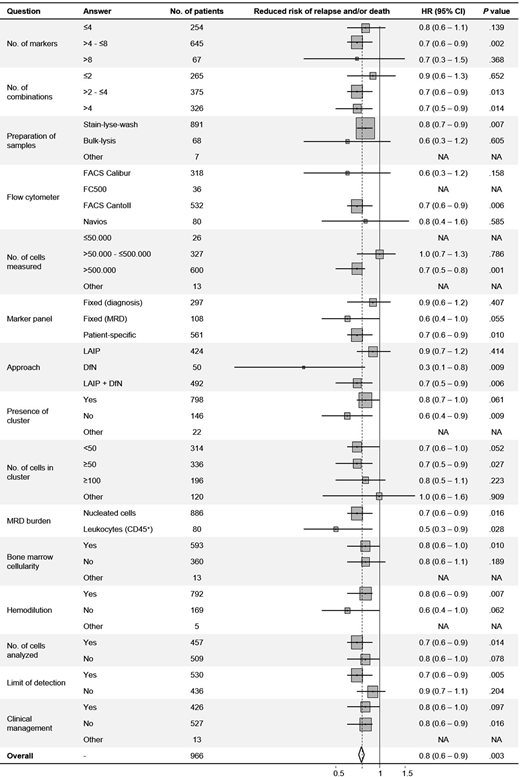
Forty-nine of the 60 hospitals (82%) responded to the survey on questions regarding the measurement of MRD using MFC in the PETHEMA LMA 1999, 2007 and 2010 protocols, providing information corresponding to 966 of the 1,076 (90%) patients regarding the number of markers, preparation of samples, instruments, approach (ie, LAIP, DfN or LAIP+DfN), number of cells to define a cluster, etc. The survey revealed significant heterogeneity intra- and inter-protocols that reflected improvement in MFC assessment of MRD over time, in the absence of harmonization nor standardization at the national level. Accordingly, we investigated if the heterogeneity in methodological, interpretation and reporting aspects of MFC based MRD testing were hampering its ability to predict outcome independently of other patient and treatment related factors. Strikingly, our results showed that except for the denominator used to calculate MRD burden (ie, total nucleated cells vs leukocytes), lack of standardization in all other parameters had an impact on the ability of MFC to predict outcomes in AML (Figure). Namely, panels with ≤4 markers or ≤2 combinations failed to identify patients with significantly different RFS according to MRD status, and MFC-based MRD monitoring was prognostic only when >500,000 cells were measured. Only MRD assessment using patient-specific panels was predictive of outcome.
Conclusions: We report here one of the largest studies investigating the role of MRD monitoring using MFC. Our results confirmed that detection of MRD identifies patients in CR/CRi with inferior survival, but uncovered that decentralized MRD testing lacks significance when compared to other baseline risk factors and in the context of risk-adapted post-consolidation strategies. Thus, while this study demonstrated that "real-world" decentralized assessment of MRD using MFC does provide prognostic information in AML patients at first remission, our results question its readiness for risk stratification towards clinical decisions outside trials, at least until adequate standardization of this technique is achieved.
Paiva:SkylineDx: Consultancy; Takeda: Consultancy, Honoraria, Research Funding; Roche: Research Funding; Adaptive: Honoraria; Amgen: Honoraria; Janssen: Consultancy, Honoraria; Karyopharm: Consultancy, Honoraria; Kite: Consultancy; Celgene: Consultancy, Honoraria, Research Funding, Speakers Bureau; Sanofi: Consultancy, Honoraria, Research Funding. Alonso Dominguez:Celgene: Research Funding; Incyte: Research Funding; Pfizer: Research Funding. Martinez-Lopez:Janssen: Speakers Bureau; Altum: Membership on an entity's Board of Directors or advisory committees, Patents & Royalties; Hosea: Membership on an entity's Board of Directors or advisory committees, Patents & Royalties; Roche: Speakers Bureau; Amgen: Speakers Bureau; Takeda: Speakers Bureau; Vivia Biotech: Honoraria; Novartis: Research Funding; BMS: Research Funding, Speakers Bureau; Incyte: Research Funding, Speakers Bureau. Sossa:Astellas: Honoraria; Roche: Honoraria; Takeda: Honoraria; Novo: Honoraria. San-Miguel:Roche, AbbVie, GlaxoSmithKline, and Karyopharm: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb, Celgene, Novartis, Takeda, Amgen, MSD, Janssen, and Sanofi: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal